Apr 8 2015
NIBIB-funded researchers have developed a highly effective sensor system to improve the quality of clinical breast examinations by physicians. The training system addresses a critical need for physicians to develop the technique and skill necessary to consistently detect the presence of breast lesions during a clinical breast exam (CBE).
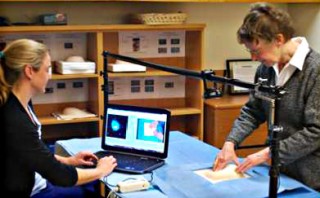 Data collection set-up showing a participant palpating the breast model and the simultaneous video and pressure recordings captured on the technician’s computer screen. From NEJM, Laufer S, et al. Sensor technology in assessments of clinical skill, 2015 Feb 19;372(8):784-6, Copyright © (2015) Massachusetts Medical Society.
Data collection set-up showing a participant palpating the breast model and the simultaneous video and pressure recordings captured on the technician’s computer screen. From NEJM, Laufer S, et al. Sensor technology in assessments of clinical skill, 2015 Feb 19;372(8):784-6, Copyright © (2015) Massachusetts Medical Society.
To improve training, the device incorporates a sensor that indicates when a physician is palpating (pressing) with adequate force necessary to detect a lump in the breast.
When doctors are training to perform a CBE, they palpate against the breast, checking for hard or irregular lumps that may be tumors. Currently, an experienced physician observer judges whether the trainee is performing the exam correctly, which involves covering the entire breast and palpating with enough pressure to feel any irregularities. The team conducted the study to determine whether the addition of sensor technologies, which measure the amount of pressure used by a trainee, would improve upon the observer-based training. The results of the study were published in the February 19 issue of the New England Journal of Medicine.
Principle investigator of the study, Carla Pugh, M.D., Ph.D., director of patient safety and education at the University of Wisconsin Hospital and Clinics, and her research team, used previously validated, sensor-enabled breast models to measure CBE technique. The sensors in the breast models provide a visual map on a computer monitor, which indicates the amount of pressure exerted by a trainee performing an exam, across the entire area of the breast model. The amount of pressure is displayed as colors seen on the map of the test breast, with blue being low palpation pressure and red being the highest palpation pressure.
Five hundred and fifty three practicing physicians performed a CBE on four sensor-enabled breast models, each with a mass of different density located in different areas of the breast. The masses represent potential tumors. Two of the models contained masses near the surface of the breast while two contained masses at the back of the breast against the chest wall.
Data were collected using simultaneous video and sensor recordings of the amount of pressure applied during the CBE by participants who successfully found the mass and those who failed to identify the mass. Analysis of the sensor data revealed that 15% of the physicians tested were using a technique that did not detect the deep tissue lesions near the chest wall planted in two of the four breast models. “The results clearly indicated that the palpation force used by each physician during CBE cannot be reliably measured by human observation,” says Pugh.
Sensor Technology in Assessments of Clinical Skill
The data collected with the sensor technology revealed that when physicians palpated with a force below 10 newtons (a measurement of force) they were able to find the superficial masses in the breast models, but missed the deeper ones located at the chest wall. The optimal amount of force that allowed physicians to detect the deeper masses was between 12 and 17 newtons.
As the director of patient safety and education, Pugh sees this sensor technology as an excellent example of the potential for significantly improved training for health care professionals. “There are huge opportunities for better information that can empower physicians and patients,” says Pugh.
The ultimate goal for Pugh and her team at UW is for the integration of technologies like sensors into clinical-skills training, assessment and credentialing. “This is an outstanding example of a novel application of sensor technology to a critical women’s health issue,” says Grace Peng, Ph.D., Director of the NIBIB Program in Medical Simulation. “Millions of women could potentially benefit from the use of this system, which holds tremendous possibilities for earlier, more accurate diagnosis of breast cancer, ultimately leading to improved treatment of the disease.”