Diabetes is one of the most severe and pervasive diseases globally. It affects nearly a third of the population in certain nations and poses significant financial burdens for treatment, and its prevalence is increasing worldwide.
In the United States alone, the rate of diabetes diagnoses among adults has doubled over the past two decades.
Although obtaining precise figures can be challenging, the numbers are substantial. According to the World Health Organization (WHO), there are more than 420 million individuals worldwide afflicted by diabetes, with an additional 370 million at risk of developing type 2 diabetes.
The International Diabetes Federation (IDF) states that approximately 537 million people across the globe have diabetes. Cases have been on the rise in recent decades, and the IDF predicts a 46% increase, reaching 783 million people with diabetes by 2045.
This growth is primarily driven by the escalating prevalence of type 2 diabetes in all countries.
Factors contributing to this trend likely include a combination of economic development and urbanization, often leading to lifestyles with higher diabetes risks. Additionally, an aging global population increases the likelihood of developing and living with diabetes for longer durations.
While a cure for diabetes remains elusive, longer lifespans signify progress in medical care. Early detection, improved self-management solutions, and effective diabetes treatment have resulted in extended survival rates, thereby contributing to the rising prevalence of the disease.
Understanding Diabetes
Improving current understanding of the disease has been a crucial factor in enhancing outcomes.
Diabetes mellitus and its symptoms have been known for thousands of years, with references found in Egyptian papyri, ancient Indian and Chinese medical literature, and the works of ancient Greek and Arab physicians.
However, it was not until the 19th century that an understanding of the underlying causes advanced significantly, leading to the extraction of insulin from the pancreas in 1921 and ushering in a new era of medical treatment.
Presently, diabetes is recognized as a chronic health condition that impairs the body’s ability to convert food into glucose - the sugar that nourishes our cells. The hormone insulin is required to facilitate the transfer of glucose from the bloodstream into the cells.
In Type 1 diabetes, the immune system targets and attacks the insulin-producing cells in the pancreas, resulting in limited or non-existent production of the hormone. Although its precise cause remains unknown, it is typically diagnosed at a younger age.
On the other hand, Type 2 diabetes usually develops later in life and is more commonly attributed to lifestyle factors such as diet and exercise, although genetic factors also play a significant role.
Gestational diabetes, the third type, affects pregnant women and typically persists until the birth of the baby. In both Gestational and Type 2 diabetes, the cells in the body become resistant to insulin, leading to its less effective utilization.
Whether the body produces insufficient insulin or fails to use it effectively, the outcome is an accumulation of excessive blood sugar in the bloodstream. Over time, this can lead to a wide range of severe health complications, including heart disease, vision loss, and kidney disease.
Diagnosing Diabetes
Doctors have started screening patients for diabetes. A new term, “prediabetes,” has been introduced to describe the stage where blood sugar levels are elevated but have not progressed to full-blown diabetes.
For individuals falling into this category, doctors advise incorporating exercise and dietary modifications. In the absence of any improvement in blood sugar levels, doctors may consider initiating medication.
With the introduction of a new blood test called HbA1C, diagnosing diabetes without the requirement of a 12-hour fast has become more convenient.
The American Diabetes Association recommended this test for routine screening back in 2010, as it provides a much more reliable method to detect diabetes early. Consequently, diabetes is being identified at an earlier stage, leading to the diagnosis of younger individuals.
Managing Diabetes at Your Fingertips
Today, individuals can lead long and healthy lives despite having diabetes, but certain requirements accompany it.
While some individuals with Type 2 and Gestational diabetes can manage their condition through diet and exercise, the majority of those living with diabetes rely on various methods to monitor their condition, followed by administering insulin shots or infusions to maintain optimal levels.
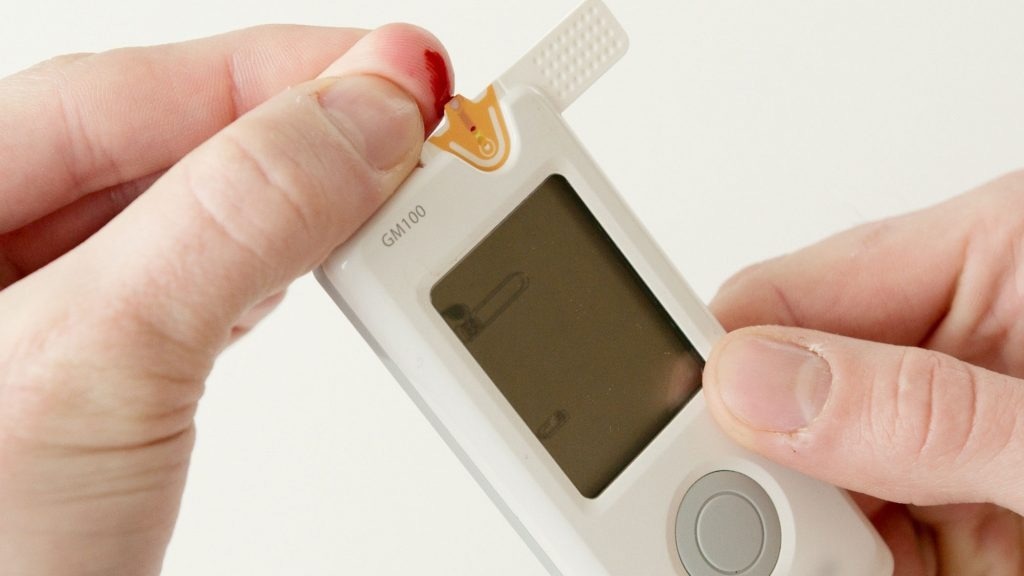
Image Credit: Teledyne Judson Technologies
Two important ways of monitoring are levels of glycated hemoglobin, which requires a blood test at a doctor’s office, and blood glucose, which can be done by a patient in their home. The measuring of blood glucose allows the patient to figure out how much insulin they need and when.
By measuring blood glucose, patients can determine the required insulin dosage and appropriate timing for administration.
This type of self-management can yield notable benefits, including the reduction of blood sugar levels, symptoms, overall mortality risk, and healthcare expenses. Moreover, staying within the target range can help enhance energy levels and mood.
Failing to achieve the target can lead to long-term effects, as well as immediate unpleasant symptoms associated with low blood sugar, such as shaking, sweating, nervousness or anxiety, dizziness, and irritability or confusion. These symptoms can further complicate the process of seeking assistance when needed.
The challenge lies in the fact that this process can be quite burdensome. In the past, patients commonly used a glucometer, which involved pricking the fingertip to obtain a small blood sample and measuring its sugar content.
While this enzyme-based method is highly accurate, it often causes skin irritation with frequent use. Additionally, the test strips are designed for single use only and can become costly over time.
Digital readers may have initial expenses that hinder accessibility, particularly in lower- and middle-income countries.
The frequency of testing varies depending on the patient and the type of diabetes but generally requires several daily measurements, including upon waking up, before consuming any food or beverages, before regular meals, and at bedtime.
Testing infrequently, even 2-3 times a day, fails to represent glucose levels throughout the day accurately. Consequently, patients often discontinue monitoring and treatment or make ill-informed decisions concerning their health due to these combined factors.
Managing Diabetes with Implantable Imaging Solutions
An alternative is necessary. A newer and increasingly popular approach entails the use of a continuous glucose monitor (CGM), which offers real-time information regarding blood sugar levels.
These devices measure at frequent intervals, and a notification system can instantly alert patients when their glucose levels are too high or too low.
Managing metabolic diseases involves the continuous monitoring of eating habits, diet, physical exercise, and sleep.
Consistent data over time from devices like CGMs can be valuable in assisting patients and healthcare professionals in comprehending physiological responses to nutrition, physical activity, and patterns in glucose control.
Collecting more data across patients also opens up significant opportunities, such as employing database-driven algorithms, multimodal information processing, and trend analysis, which can contribute to better predictive alerts and novel approaches to individual health management.
Detecting glucose levels in the blood, within a living human body, in real-time poses challenges. Factors like temperature changes and contact pressure can influence imaging, especially considering that reflected glucose signals are susceptible to strong absorption and weak intensity, thereby affecting accuracy.
One approach involving an implantable device utilizes a near-infrared (NIR) imaging sensor assisted by a fluorescent dye. However, this approach has a disadvantage in that the fluorescence is temporary, with commercial solutions lasting only a few months.
There have been proposals for electromagnetic sensors that can be implanted beneath the skin and can track minute changes in blood glucose by measuring alterations in how the blood holds an electrical charge.
Nevertheless, near-infrared imaging appears to be the most promising option as it can reveal glucose-dependent intensity variations caused by spectral absorption when illuminated and the reflectance changes with blood glucose variations.
The challenge today lies in determining which types of sensors to use in implantable devices to ensure accurate and reliable measurements.
Optical spectroscopic methods, particularly near-infrared (NIR) absorption spectroscopy, have shown potential in identifying glucose-specific features amidst various confounding signals. However, this imaging approach is non-invasive and impractical for an implantable device.
In addition to the sensor-related challenges, the design of the complete device presents its own complications.
If the device is too large, it may cause discomfort for patients. The materials used must be biologically compatible, as solid-state materials like silica can lead to infections or elicit immune reactions as foreign bodies.
Despite these challenges, many researchers are working on new solutions.
A recent feasibility study partially funded by the EU examined a subcutaneous multi-metabolite sensor, indicating that a CGM system could overcome the limitations of existing devices by offering a solution that remains inconspicuous on the patient’s body and requires minimal patient input.
The sensor demonstrates reliable measurement of glucose levels, as well as metabolic indicators such as ketones and lactate. Together, these indicators provide more comprehensive information on fat metabolism and physical activity, aiding in the prediction of dangerously low or high glucose levels.
Looking Forward
Effective management of diabetes has the potential to decrease healthcare expenses and mitigate the numerous medical complications associated with the condition for millions of individuals.
The costs are substantial, with healthcare expenditures for diabetes surpassing USD 760 billion annually on a global scale, and this figure continues to rise, and nearly 40% of this expenditure is attributed to the United States alone.
Organizations such as the Rand Corporation and the Mayo Clinic have raised the alarm about the high costs of diabetes care and related costs. Thus, a combination of new solutions and better technology will be needed to face this growing problem in the future.
This information has been sourced, reviewed and adapted from materials provided by Teledyne Judson Technologies.
For more information on this source, please visit Teledyne Judson Technologies.