Feb 9 2016
Scientists at the University of Southampton are to develop and trial a new wearable technology to help people who have had a stroke recover use of their arm and hand.
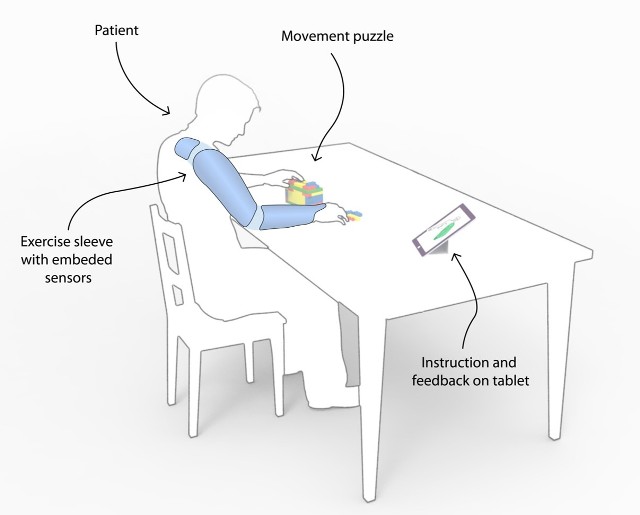
Led by Professor Jane Burridge, the team will create a wireless sleeve, which will provide automatic, intelligent information about muscle movement and strength while patients practice every-day tasks at home.
The data will be available on a computer tablet to enable patients to review their progress as well as to allow therapists to tailor their rehabilitation programme.
The two-year project has been funded with a grant of just under £1 million from the National Institute for Health Research (NIHR) through its Invention for Innovation (i4i) programme and is a collaboration between the University of Southampton and Imperial College London, two medical technology consultancies; Maddison and Tactiq and NHS Trusts in Bristol and Portsmouth.
Jane Burridge, Professor of Restorative Neuroscience at Southampton, comments: "About 150,000 people in the UK have a stroke each year and, despite improvements in acute care that results in better survival rates, about 60 per cent of people with moderate to severe strokes fail to recover useful function of their arm and hand.
"Stroke rehabilitation is increasingly home-based, as patients are often discharged from hospital after only a few days. This policy encourages independence and avoids problems associated with prolonged hospital stays. However, some patients struggle to carry out the exercises and they may question whether what they are doing is correct. Similarly therapists don't have objective measurements about their patients' muscle activity or ability to move. Rehabilitation technologies like our sleeve will address problems faced by both patients and therapists."
The wearable technology is the first to incorporate mechanomyography (MMG) microphone-like sensors that detect the vibration of a muscle when it contracts, and inertial measurement units (IMU), comprising tri-axial accelerometers, gyroscopes and magnetometers that detect movement. Data from the two types of sensors will be put together and then data that is not needed, for example outside noise, will then be removed from the muscle signal.
The feedback to patients will be presented on a user-friendly computer interface as an accurate representation of their movement, showing them how much they have improved.
The same sleeve and computer tablet technology, but using different software and user-interfaces, will provide therapists with information to help them diagnose specific movement problems, and inform their clinical decision-making, monitor progress and therefore increase efficiency and effectiveness of therapy.
Professor Burridge adds: "We hope that our sleeve will help stroke patients regain the use of their arm and hand, reduce time spent with therapists and allow them to have the recommended 45 minutes daily therapy more flexibly.. It will also be used to assess patients' problems accurately as well as more cheaply and practically than using laboratory-based technologies."
The team, which includes members who themselves have suffered strokes, are working with medical device consultancies, Maddison and Tactiq to develop wearable prototypes and graphical user interfaces which can then be trialled with patients from two NHS sites. They will test the user interfaces, wireless connectivity and examine how easy the sleeve is to wear. The potential cost savings to the NHS will also be examined.