Oct 13 2016
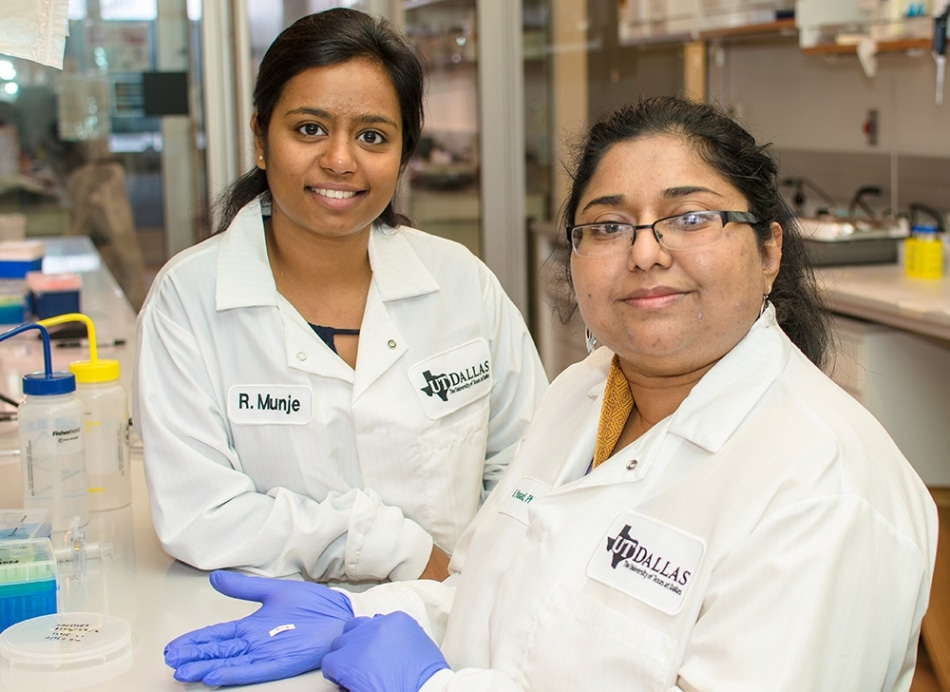 Dr. Shalini Prasad (right), professor of bioengineering at UT Dallas, and doctoral student Rujuta Munje designed a wearable, flexible biosensor that can reliably detect and quantify glucose from very small amounts of human sweat. Credit: University of Texas
Dr. Shalini Prasad (right), professor of bioengineering at UT Dallas, and doctoral student Rujuta Munje designed a wearable, flexible biosensor that can reliably detect and quantify glucose from very small amounts of human sweat. Credit: University of Texas
A team of researchers from The University of Texas, Dallas, are developing a wearable device capable of controlling an individual’s glucose level through perspiration on the skin.
The journal Sensors and Actuators B: Chemical, recently featured a study where Dr. Shalini Prasad, professor of bioengineering in the Erik Jonsson School of Engineering and Computer Science, and her co-authors illustrated the potential of a biosensor they created in order to detect and quantify glucose in an individual’s sweat in a reliable manner.
Previously, the team had illustrated that their technology was capable of identifying cortisol in perspiration.
Self-monitoring of blood sugar, or blood glucose is considered to be a vital part to control the conditions of diabetics and those individuals at the risk of becoming diabetic.
“Fitness trackers that monitor heart rate and step count are very popular, but wearable, non-invasive biosensors would be extremely beneficial for managing diseases,” said Prasad, the Cecil H. and Ida Green Professor in Systems Biology Science.
Standard home-use blood glucose monitors need a user to obtain a small blood sample, which is often done with a prick of the finger many times throughout the day. However, glucose in the small amount of ambient sweat on an individual’s skin is detected by the UT Dallas textile-based sensor.
In our sensor mechanism, we use the same chemistry and enzymatic reaction that are incorporated into blood glucose testing strips. But in our design, we had to account for the low volume of ambient sweat that would be present in areas such as under a watch or wrist device, or under a patch that lies next to the skin.
Dr. Shalini Prasad, University of Texas
Prasad stated that researchers who work with sweat often use iontophoresis, which is a process that sends an electric current via the skin in order to generate sufficient perspiration for sensing experiments. The team used an alternative ideal for small amounts of sweat as the process of iontophoresis could cause burns and rashes on the skin.
The design developed by the team works with sweat volumes less than a microliter, which is the exact volume of liquid that would fit in a cube, which is the size of a salt crystal.
A real-time response in the form of a digital readout is also provided by the technology.
Prasad with Rujuta Munje, bioengineering doctoral student and chief author of the journal article, developed electronic elements by integrating an off-the-shelf polymer-based textile material in their glucose sensor and using UT Dallas clean-room facilities. The prototype is a flexible, small, rod-shaped device that is about an inch long.
We used known properties of textiles and weaves in our design. What was innovative was the way we incorporated and positioned the electrodes onto this textile in such a way that allows a very small volume of sweat to spread effectively through the surface.
Dr. Shalini Prasad, University of Texas
Standard blood glucose testing strips also comprise of a molecule that eventually amplifies the signal obtained from the chemical reactions on the strip sufficient to register electronically on a monitoring device. Prasad further stated that those molecules can become irritating if used in a device that is used next to the skin. This indeed poses another challenge.
Prasad and Munje further altered the textile material’s surface topography in order to ensure that such a small amount of sweat would produce a strong enough signal.
“Our modifications allow this material to entrap glucose oxidase molecules, which effectively amplifies the signal,” Prasad said. “We did it this way because we are thinking about possible commercialization — to make these, we need a fabrication process that is not complex.”
Prasad and Munje were also able to demonstrate the fact that the chemistry of an individual’s sweat changes throughout the day.
“Glucose is a tricky molecule to monitor because other factors can confound a signal,” Prasad said. “For example, the pH, or acidity, of your sweat can vary greatly depending on the circumstances.”
She highlighted that when individuals are under stress or exercise, the level of other compounds present in the sweat, such as lactic acid or cortisol, also change, and these can interfere with the detecting process of glucose.
“We have shown that with our technology, we address three critical issues: low volume of ambient sweat, interference from other compounds and pH swings,” Prasad said.
Prasad and Munje used samples of human sweat from donors to test their prototype.
Even though a consumer product based on the technology is yet to be developed, the concept was formed with scaled-up production and commercialization in mind.
At this point, we are thinking of this sensor as something you use for a day and toss out, and we believe it could easily be incorporated into existing consumer electronics platforms. We’re very excited about the potential for licensing this technology.
Dr. Shalini Prasad, University of Texas
The work was supported by the Cecil H. and Ida Green endowed fellowship at UT Dallas.
Researchers at UT Dallas and also from other places have analyzed whether glucose detected in other bodily fluids, such as tears and urine, might be used to monitor glucose levels, further preventing the requirement for invasive blood draws. For example, Google is examining a smart contact lens that has been developed for measuring the levels of glucose in tears.
The Centers for Disease Control and Prevention assume that 86 million people in the United States have prediabetes and 29 million have diabetes.