Aug 23 2018
Using a new biosensor, researchers can now track oxygen levels in real time in “organ-on-a-chip” systems, making it possible to guarantee that such systems more closely imitate the function of real organs. This is crucial if organs-on-a-chip hope to realize their potential in applications such as drug and toxicity testing.
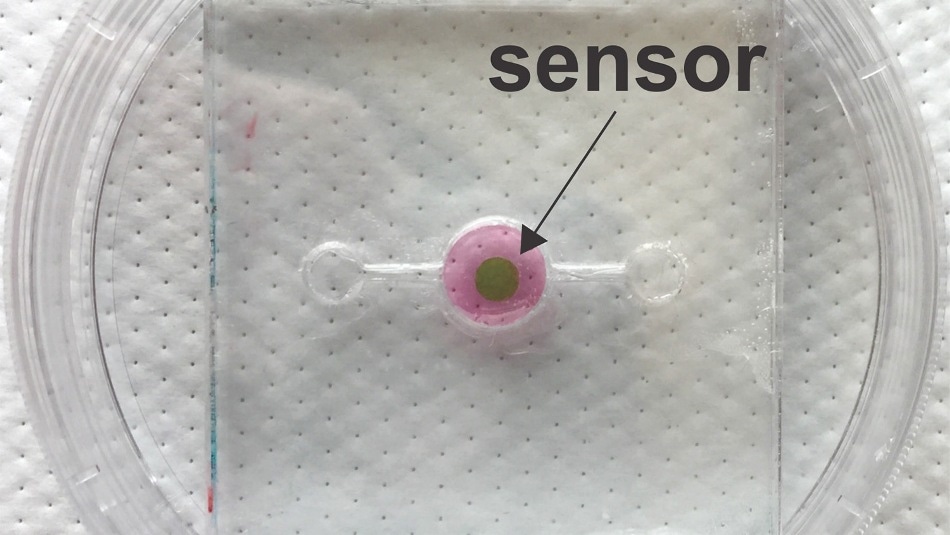 A new biosensor allows researchers to track oxygen levels in real time in 'organ-on-a-chip' systems, making it possible to ensure that such systems more closely mimic the function of real organs. This is essential if organs-on-a-chip hope to achieve their potential in applications such as drug and toxicity testing. The biosensor was developed by researchers at NC State University and UNC-Chapel Hill. (Image credit: Michael Daniele)
A new biosensor allows researchers to track oxygen levels in real time in 'organ-on-a-chip' systems, making it possible to ensure that such systems more closely mimic the function of real organs. This is essential if organs-on-a-chip hope to achieve their potential in applications such as drug and toxicity testing. The biosensor was developed by researchers at NC State University and UNC-Chapel Hill. (Image credit: Michael Daniele)
The organ-on-a-chip concept has garnered substantial attention from scientists for nearly a decade. The idea is to develop small-scale, biological structures that imitate a specific organ function, such as conveying oxygen from the air into the bloodstream in the same manner as a real lung. The goal is to use these organs-on-a-chips - also called microphysiological models - to accelerate high-throughput testing to measure toxicity or to assess the effectiveness of new drugs.
Although organ-on-a-chip research has made momentous advances in the last few years, one hurdle to the use of these structures is the lack of tools engineered to truly retrieve data from the system.
“For the most part, the only existing ways of collecting data on what’s happening in an organ-on-a-chip are to conduct a bioassay, histology, or use some other technique that involves destroying the tissue,” says Michael Daniele, corresponding author of a paper on the new biosensor. Daniele is an assistant professor of electrical engineering at North Carolina State University and in the Joint Department of Biomedical Engineering at NC State and the University of North Carolina, Chapel Hill.
What we really need are tools that provide a means to collect data in real time without affecting the system’s operation. That would enable us to collect and analyze data continuously, and offer richer insights into what’s going on. Our new biosensor does exactly that, at least for oxygen levels.
Michael Daniele, Corresponding Author
Oxygen levels differ extensively across the body. For instance, in a healthy adult, lung tissue contains an oxygen concentration of about 15%, while the inner lining of the intestine is about 0%. This matters because oxygen directly influences tissue function. If one wants to know how an organ is going to act normally, “normal” oxygen levels must be maintained in the organ-on-a-chip while conducting experiments.
“What this means in practical terms is that we need a way to monitor oxygen levels not only in the organ-on-a-chip’s immediate environment, but in the organ-on-a-chip’s tissue itself,” Daniele says. “And we need to be able to do it in real time. Now we have a way to do that.”
The core to the biosensor is a phosphorescent gel that discharges infrared light after being exposed to infrared light. Imagine it as an echoing flash. But the lag time between when the gel is exposed to light and when it discharges the echoing flash differs, based on the amount of oxygen in its environment. If the oxygen is more, the lag time is shorter. These lag times last for just microseconds, but by checking those times, scientists can calculate the oxygen concentration down to tenths of a percent.
For the biosensor to function, scientists must add a thin layer of the gel into an organ-on-a-chip during its assembly. As infrared light can pass via tissue, scientists can use a “reader”—which discharges infrared light and measures the echoing flash from the phosphorescent gel—to track oxygen levels in the tissue repetitively, with delay times measured in the microseconds.
The research team that created the biosensor has tested it successfully in 3D scaffolds using human breast epithelial cells to model both cancerous and healthy tissue.
One of our next steps is to incorporate the biosensor into a system that automatically makes adjustments to maintain the desired oxygen concentration in the organ-on-a-chip. We’re also hoping to work with other tissue engineering researchers and industry. We think our biosensor could be a valuable instrument for helping to advance the development of organs-on-a-chip as viable research tools.
Michael Daniele, Corresponding Author
The paper, “Integrated phosphorescence-based photonic biosensor (iPOB) for monitoring oxygen levels in 3D cell culture systems,” is reported in the journal Biosensors and Bioelectronics. The paper’s first author on is Kristina Rivera, a Ph.D. student in the Joint Department of Biomedical Engineering. The paper was co-authored by Ashlyn Young and Patrick Erb, Ph.D. students in the Joint Department of Biomedical Engineering; Vladimir Pozdin, a postdoctoral researcher at NC State; Natalie Wisniewski of Profusa, Inc.; and Scott Magness, an associate professor at UNC and in the Joint Department of Biomedical Engineering.
The research was done in partnership with NC State’s National Science Foundation-funded Advanced Self-Powered Systems of Integrated Sensors and Technologies (ASSIST) Center under grant EEC1160483.