Oct 1 2019
Small, non-invasive patches worn on the skin can exactly detect the levels of medication in a patient’s system, matching the precision of existing clinical procedures.
 (Image credit: © Imperial College London)
(Image credit: © Imperial College London)
In a small-scale clinical evaluation, scientists at Imperial College London have demonstrated for the first time how microneedle biosensors can be used to track the changing concentration of antibiotics.
Their findings, reported recently in The Lancet Digital Health, reveal that the sensors allow real-time tracking of variations in antibiotic concentration in the body, with comparable results to those acquired from blood tests.
The researchers believe the technology could transform how patients with critical infections are treated by showing how rapidly their bodies “use up” medications that are administered. The scientists added that if future progress and testing prove successful and the technology reaches the hospital, it could help to bring down costs for the NHS, decrease drug-resistant infections, enhance treatment for patients with serious infections, and optimize the management of less serious ones.
According to the researchers, biosensors could bring down the need for blood sampling and examination as well as provide more efficient and personalized drug delivery that could possibly be delivered beyond the hospital setting for outpatients.
Real-Time Monitoring
Microneedle biosensors hold a great potential for monitoring and treating the sickest of patients. When patients in hospital are treated for severe bacterial infections the only way we have of seeing whether antibiotics we give them are working is to wait and see how they respond, and to take frequent blood samples to analyse levels of the drugs in their system—but this can take time.
Dr Timothy Rawson, Study Lead, Department of Infectious Disease, Imperial College London
Dr Timothy Rawson added, “Our biosensors could help to change that. By using a simple patch on the skin of the arm, or potentially at the site of infection, it could tell us how much of a drug is being used by the body and provide us with vital medical information, in real-time.”
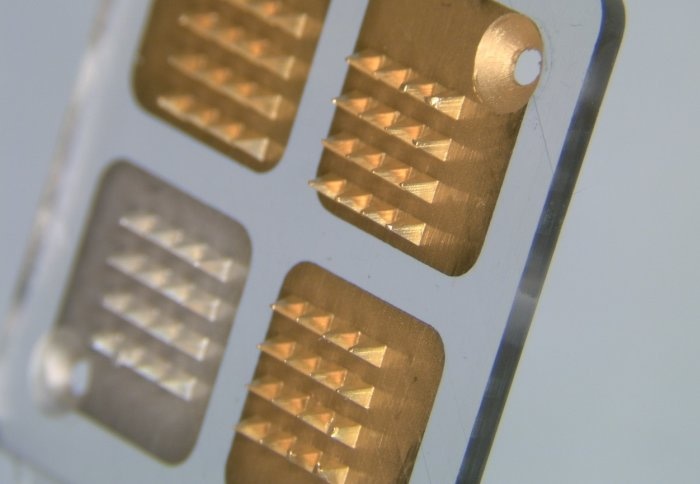
Microneedle biosensors use a sequence of microscopic “teeth” to penetrate the skin and sense variations in the fluid between cells. These teeth serve as electrodes to spot variations in pH and can be coated with enzymes that react with a preferred drug, changing the local pH of the nearby tissue if the drug is present.
The technology has been used for nonstop tracking of blood sugar, but for the first time, the Imperial team has demonstrated its potential for use in monitoring variations in drug concentrations.
In a small proof-of-concept experiment, the Imperial researchers trialed the sensors in 10 healthy patients who were administered doses of penicillin. Sensor patches measuring 1.5 cm2 were positioned on their forearms and linked to monitors, with measurements taken regularly — from 30 minutes before being given oral penicillin, to four hours afterward. Blood samples were collected at the same time points for comparison purposes.
Data gathered from nine patients showed that the sensors could precisely detect the varying concentration of penicillin in patients' bodies. The scientists learned that while penicillin concentrations differed extensively from one patient to another, the general readings from the biosensors were akin to those from blood samples — displaying a noticeable decrease in drug concentration over time.
According to the researchers, the early findings are positive, but they explain the study is restricted by the very small sample size which was only tested on a single antibiotic, in patients who were healthy.
Optimizing Antibiotic Dosage
The scientists explain that together with additional testing in larger patient groups to reinforce the preliminary findings, they will explore to see how the sensors could help to enhance the dosing of penicillin and related antibiotics.
They further stated that the sensors could form the foundation of a “closed loop system,” similar to an insulin pump — where antibiotics are given to patients and levels continuously checked to ensure they receive an adequate dose.
This small, early-stage trial has shown that the sensor technology is as effective as gold standard clinical analysis in detecting changes to the concentrations of penicillin in the human body. When further developed, this technology could prove critical for the monitoring and treatment of patients with severe infections. More widely it could be used to monitor many other drugs and personalise treatment in many diseases.
Tony Cass, Professor, Department of Chemistry, Imperial College London
The technology was made possible through research backed by funding from the National Institute for Health Research (NIHR) and Fondation Merieux. Volunteers were enlisted and treated at the NIHR Imperial Biomedical Research Centre at Imperial College Healthcare NHS Trust. This joint effort will be advanced further through Imperial’s National Centre for Antimicrobial Research and Optimization (CAMO).
Professor Alison Holmes, from Imperial's Department of Infectious Disease and director of the NIHR Health Protection Research Unit in HCAI and AMR at Imperial and the CAMO, said, “This technology is an example of the close collaboration between scientists, medics and engineers going on in institutions across the UK, which could change the way we treat patients. Antibiotic resistance and drug-resistant infections are among the biggest threats to human health in the world today.”
Technological solutions such as our microneedle biosensor could prove crucial in improving how we use and protect the arsenal of life-saving antibiotics we have available to treat patients. Ultimately, these types of collaborative, multidisciplinary solutions could lead to earlier detection and better treatment of infections, helping to save more lives and protect these invaluable medicines for generations to come.
Alison Holmes, Professor, Department of Infectious Disease, Imperial College London
The study was sponsored by the NIHR Imperial Biomedical Research Centre and Fondation Mérieux and supported by the infrastructure of the NIHR Health Protection Research Unit in HCAI and AMR at Imperial and the NIHR Clinical Research Facility at Imperial.