Reviewed by Lexie CornerMar 20 2024
For decades, diabetes patients have depended on finger pricks to draw blood or adhesive microneedles to measure and manage their blood sugar levels. These techniques can lead to infection, inflammation, itching, and pain.
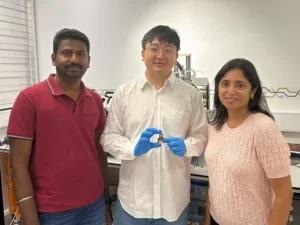
Image Credit: Australian Research Council Center of Excellence for Transformative Meta-Optical Systems
Researchers at TMOS, the Australian Research Council Center of Excellence for Transformative Meta-Optical Systems, have made significant progress toward removing this discomfort.
Their RMIT University team has uncovered new facets of the infrared signature of glucose and has utilized this knowledge to create a 5 mm diameter miniature optical sensor that may one day be utilized for continuous non-invasive glucose monitoring in diabetes treatment.
As non-invasive glucose sensing offers the potential for painless monitoring, it has been a focus for nearly 30 years. Although reports of optical glucose sensing techniques exist, they are not suitable for routine patient use due to the need for complex optical instrumentation found in laboratories.
The main difficulty in developing an inexpensive, wearable optical glucose test has been shrinking the device and separating the near-infrared (NIR) water absorption peaks from the glucose signals. Essentially, distinguishing between water and glucose in the blood has proven to be nearly impossible until now.
The team has discovered four infrared peaks in glucose that enable sensitive and selective identification in biological and aqueous environments. This is the first of its kind research, and it was published in the journal Advanced Sensor Research. To carry out pre-clinical and clinical research and advance the development of wearable optical glucose sensors, the team is eager to work with academic and industrial partners.
The team has developed a compact glucose sensor operating on a 1600–1700 nm waveband, equipped with Bluetooth functionality and powered by a coin battery. This design facilitates continuous glucose monitoring. This small sensor has proven to be effective in measuring blood plasma glucose levels, which range from 50 to 400 mg/dL in humans, with a sensitivity and detection limit that is similar to larger, lab-based sensors. Due to its small size, it might eventually be included in smartwatches and other painless wearable health trackers.
Until now, there is no consensus on the unique spectroscopic signature of glucose, largely because the O-H bonds targeted in near-infrared (NIR) spectroscopy for glucose detection are also abundant in water. This similarity makes it challenging to distinguish between glucose and water signals, especially in complex biological fluids and tissues. We optimized spectroscopy setup and analyzed transmittance to identify peaks unique to glucose. Our discovery finally provides the information necessary to move forward with miniaturized optical glucose sensing, and we have developed a device prototype to suggest the foundation for futuristic, non-invasive glucose sensor.
Mingjie Yang, Study Lead Author and Ph.D. Scholar, RMIT
The device prototype uses circuits composed of thin-film copper coated polymide (Cu/PI), which is only 110 µ thick, and a surface-mounted device light emitting diode (SMD LED), developed using laser patterning technology. This device’s lightweight construction and mm scale make it significantly more compact than conventional benchtop spectrophotometers. Additionally, direct reading as a wearable device on human skin may be possible in the future thanks to the flexible patch-like design.
The device’s performance has been thoroughly assessed in both blood plasma and aqueous glucose solutions. The light-skin interference has been computationally analyzed to show how the SMD LED will pierce the skin. The outcomes of the simulation point to potential areas for further investigation into optical glucose sensing in clinical settings.
The non-invasive nature of optical glucose sensors has the potential to improve patient compliance, reduce discomfort, and lower the risks of infections associated with invasive glucose monitoring. With the right collaborators/partners and the right funding, this can represent an important shift towards continuous and pain-free glucose sensing.
Madhu Bhaskaran, Chief Investigator, TMOS
Wearable sensors like the one engineered by TMOS researchers at RMIT University are integral to the Centre's Meta Health Sensors Flagship Program. This program focuses on applied research dedicated to advancing meta-optical sensors for medical technology (MedTech) applications.
RMIT University has submitted a patent application regarding the optical glucose sensor technology that the group created.
Journal Reference:
Yang, M., et al. (2024) Miniaturized Optical Glucose Sensor Using 1600–1700 nm Near-Infrared Light. Advanced Sensor Research. doi.org/10.1002/adsr.202300160