.png) Interview conducted by Emily Henderson, B.Sc.Nov 16 2021
Interview conducted by Emily Henderson, B.Sc.Nov 16 2021AZoSensors talks to Dr. Marta Tessarolo about new ‘smart bandages’ which use sensor technology to non-invasively monitor wound healing.
Please introduce yourself and tell us how you got into wound healing research.
I am Marta Tessarolo a physicist specializing in organic semiconductors working at the University of Bologna collaborating with the research groups of Prof Beatrice Fraboni at the Department of Physics and Astronomy and of Prof Erika Scavetta at the Department of Industrial Chemistry. Combining our expertise, we developed several wearable organic chemical sensors.
Checking on healing wounds involves a tricky balance between being able to check the wound’s moisture levels and avoiding disruption of the healing process. How could the new ‘smart bandage’ be a solution to this problem?
A doctor commonly inspects the wound by removing the bandage, which has to then be replaced, interrupting the healing process.
With our smart bandage, doctors can wirelessly check in real-time the moisture status and decide if the bandage needs replacing, optimizing the healing process and reducing bandage waste.
Our integrated fully passive moisture sensor can be easily read with a common smartphone by just placing it close to the smart bandage. A low value of impedance is a consequence of a wet wound, comparatively, a high impedance is related to a dry wound. The optimal moisture level depends on the type of wound and its healing state.

Image Credit: Bangkoker/Shutterstock.com
Why are moisture levels so important in wound healing? What other factors affect it?
As reported by several papers in the scientific literature, the moisture level is relevant for the healing process, the optimum moisture level depending on the type of wound, its extension, and its healing state. For example, if a wound produces too much exudate, bandages have to be replaced more often to prevent maceration.
Other parameters such as pH, temperature, and concentration of several bioproducts can be used to monitor and better understand the healing process. With our research group, we are actively working on developing a fully textile biochemical sensor that is able to monitor in real-time other relevant biomarkers in biofluids, such as pH, dopamine, and adrenaline.
How does the sensor technology in the smart bandage work?
Our smart bandage exploits a simple working principle; two electrodes based on a conductive polymer are printed in a specific geometry leaving a small gap between them. If the bandage is dry the two electrodes are not in electrical contact and the measured impedance is high.
On the opposite, when a small amount of exudate wets the bandage, the conductive polymer is able to transduce ions of the biofluid into electrons that are collected by the electrodes, inducing a drastic drop in the impedance value. We implemented this principle by optimizing the sensor geometry and bandage layers composition, obtaining sensors able to reversibly operate for a wide range of exudate volumes, starting from as little as 5 microliters.
Why was choosing materials for a bandage a challenge and how did you overcome this?
The field of wound bandage materials is well developed and widespread. This research is the outcome of a collaboration with an Italian bandage company (PLASTOD spa).
Our bandages have been fabricated with materials routinely used in the bandage industry, therefore they are biocompatible and safe to use. The bandage materials have different compositions and absorption properties and we carefully selected and combined them to tune the bandage sensing performance over a very broad range of exudate volumes.
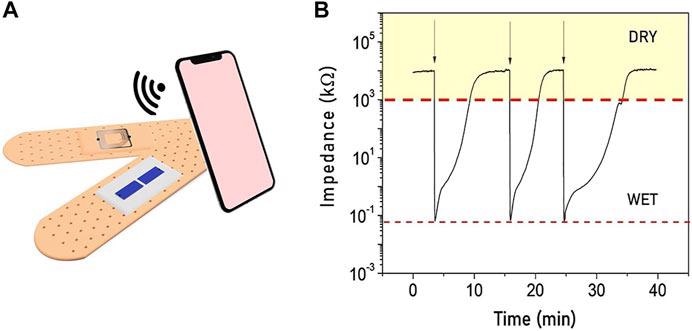
Image Credit: https://doi.org/10.3389/fphy.2021.722173
How did you test the smart bandages?
Smart bandages were tested in the laboratory with artificial exudate.
What techniques were used to create this smart bandage?
Each sensor is composed of two conductive polymers (PEDOT: PSS) electrodes. PEDOT: PSS is a water-based dispersion used as an ink to screen printed electrodes directly onto the bandage layer. The final bandage retains the typical multilayer stacked.
The wireless, fully passive, readout system consists of an RFID/NFC chip and related antenna integrated into the bandage cover with the same technology used for garment tags.
How could smart bandages improve the livelihoods of people with chronic wounds?
In real-life applications, one could foresee the use of our smart bandages for chronic wound patients that need constant monitoring of their wound state. They would simply have to draw their mobile phone near the bandage to wirelessly read the wound moisture level.
No power supply is needed at any stage. The result can be transmitted in real-time to the medical doctor that will provide appropriate support and counseling on the actions to take.

Image Credit: ARTFULLY PHOTOGRAPHER/Shutterstock.com
How could the technology be adapted to different types of wounds and what would this entail?
Different types of wounds require different types of bandages as their moisture level and their extension requires different treatments. Insert our sensor into those bandages, it is easy and the working principles it is not affected. What is needed is a trial to interpret the results and individuate the threshold signal.
Could this sort of technology be applied to other areas of medical treatment?
Smart bandages which combine moisture sensors and other biochemical sensors would be very interesting and useful to monitor sweat or other body fluids to detect the presence and concentration of relevant biomarkers for medical diagnostics but also sports activity and performance.
What is the next step for your smart bandages?
On one hand, we have a plan to test the smart bandages in real applications for several wounds and different bandages to identify relative threshold values, collecting data for a database optimizing sensor response interpretation.
On the other hand, we are developing different biochemical sensors which can be included in the smart bandage to monitor several parameters and better understand the healing process.
Where can readers find more information?
About Dr. Marta Tessarolo
Marta Tessarolo received a Ph.D. (2016) in Physics at the University of Bologna. In her career, she worked in Area Science Park – Trieste developing advanced technologies for cancer diagnostics. Then she moved to the National Research Council (CNR) in Bologna focusing her research on flexible organic solar cells.
Recently, she got a post-doc position at the University of Bologna, Department of Physics and Astronomy, and in the field of wearable textile biosensors based on polymer semiconductors. Currently, she works as a laboratory technician in the same Department. She has wrote more than 30 papers in international scientific journals, attended many international scientific conferences, and follows the technology transfer on several research projects on textile and flexible biosensors.
Disclaimer: The views expressed here are those of the interviewee and do not necessarily represent the views of AZoM.com Limited (T/A) AZoNetwork, the owner and operator of this website. This disclaimer forms part of the Terms and Conditions of use of this website.