Apr 23 2014
The task was to develop intelligent prosthetic joints that, via sensors, are capable of detecting early failure long before a patient suffers. EPFL researchers have taken up the challenge.
 © 2014 Alain Herzog
© 2014 Alain Herzog
Today, nearly 4 million people worldwide must suffer through operations to replace defective joints. In the coming years, the number of procedures on knees will multiply by 7. EPFL researchers have developed sensors, integrated into the polyethylene part of the prosthesis, that can perform a diagnosis of the interior, improving medical treatment and thereby helping patients, in some cases, avoid a new operation.
There are three leading causes of this surgical boom: the development of recreational sports that particularly affect the knee and eventually cause osteoarthritis, obesity – a sport in itself for the joint that must bear the excess weight, and lesions that are present in cartilage. Once the arthroplasty has been performed, the prosthesis set, and the operating field closed, the biggest problem for the doctor is that the only feedback is the patient’s qualitative and subjective assessment. If the prosthesis is misaligned or if it unseals, which occurs in about 20% of cases, this causes significant pain, and it is very difficult to quantify.
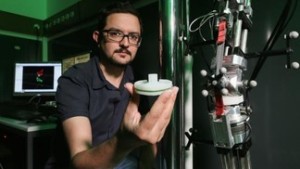
Arash Arami of the Laboratory of Movement Analysis and Measurement (LMAM) devoted part of his thesis to the question of unsealing in the prosthesis. He chose the knee because it is a complex joint that is often injured. With an algorithm he developed, he could precisely calculate the micromovements of the prosthesis and detect, via vibration, any loosening. Then, using sensors implanted in a prosthesis mounted on a mechanical knee simulator, he could demonstrate how it reacts to applied forces.
Brigitte Jolles-Haeberli, head of prosthetic knee surgery at the University Hospital of Lausanne and EPFL’s Interinstitutional Center of Translational Biomechanics, collaborated closely on this project. “Even when a prosthesis has been properly installed, some people experience persistent pain. One is at a loss for how to concretely help without resorting to painkillers or physiotherapy.” Even if it is possible to see the problems of sealing or alignment – through an x-ray coupled with a bone scan – doctors still have no way to detect the cause. “With this new information about the prosthesis, we could take preventative measures and explore other avenues of gait rehabilitation without necessarily having to resort to a new surgery.”
Five EPFL laboratories have joined in a project funded by the National Science Foundation. To help the industry integrate new tools into smart prostheses, the scientists decided to put these sensors in the middle part, which is the polyethylene insert. This material is common to all knee prostheses, regardless of manufacturer.
“It makes sense that all these inserts have more or less the same shape and therefore the same volume, and if we can instrumentalize it without touching the femoral or tibial part, it will be easier for the industry to implement. But this will not happen immediately, because we must first show how these sensors represent a real benefit for both patients as well as doctors and the industry,” concluded Kamiar Aminian who directs the LMAM.
http://www.nano-tera.ch/projects/81.php
Author: Sandy Evangelista
Source: Mediacom